Cancer treatments such as radiotherapy, chemotherapy, and surgery play a crucial role in fighting cancer. However, these treatments can have unintended consequences on the thyroid gland, leading to the development of hypothyroidism. While cancer treatments target cancer cells to slow their growth and spread, they may also damage or remove healthy tissue, including the thyroid gland. This can result in various health issues, including hypothyroidism, where the thyroid cannot produce enough hormones to function properly.
Risks of Hypothyroidism
Various cancer treatments can increase a person’s risk of developing hypothyroidism. For instance, surgery and radiation therapy directly damage or remove thyroid tissue, impairing the production of thyroid hormones. Similarly, certain chemotherapy drugs and medications can interfere with thyroid hormone production or trigger the immune system to attack the thyroid. A combination of chemotherapy and radiation therapy has been found to pose the highest risk of hypothyroidism, particularly in individuals who have had breast cancer.
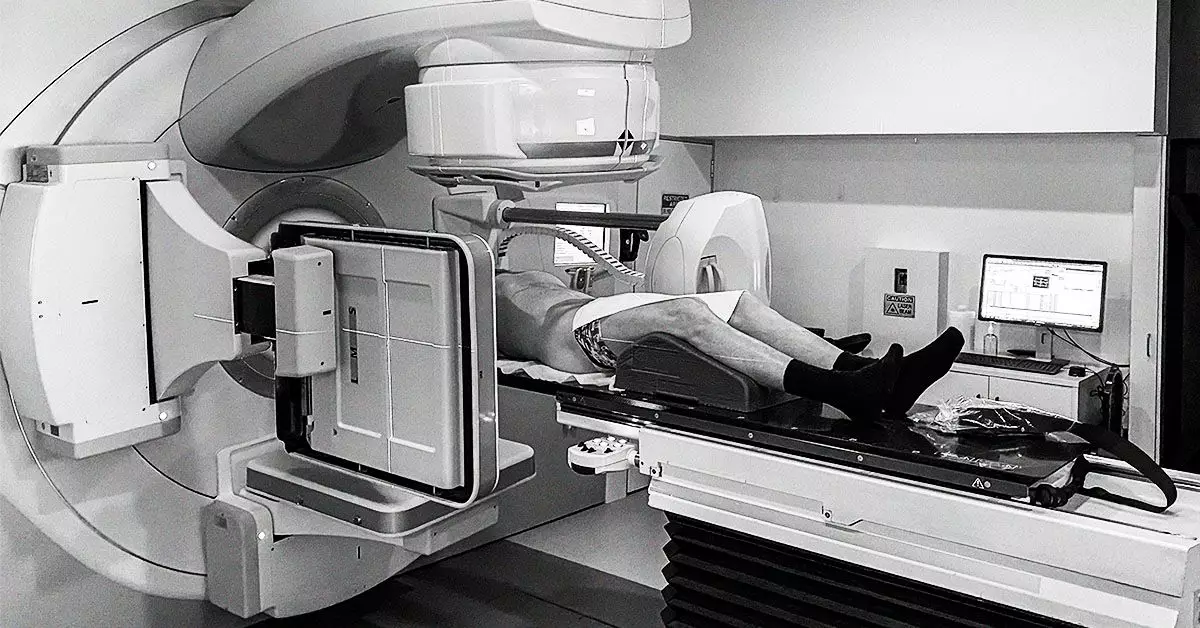
Radiation therapy, often used to treat head and neck cancers, can significantly impact thyroid health. Research indicates that up to 40-50% of individuals receiving radiation therapy may develop hypothyroidism. The thyroid gland is particularly vulnerable to radiation, leading to the destruction of thyroid tissue and hormone-producing capabilities. Factors such as the radiation dose, type of therapy, individual’s age, and sex can influence the risk of hypothyroidism following radiation treatment.
Surgery is a common treatment for thyroid cancer, often involving the removal of cancerous thyroid tissue. Depending on the extent of cancer, surgeons may remove part or all of the thyroid, resulting in decreased hormone production. This can lead to hypothyroidism post-treatment, necessitating lifelong hormone replacement therapy. Hormone therapy medications may also block thyroid-stimulating hormone, further impacting thyroid hormone levels and potentially causing hypothyroidism.
Immunotherapy, a type of cancer treatment that harnesses the immune system to fight cancer, can also affect thyroid health. Immune checkpoint inhibitors, a class of immunotherapy drugs, may cause thyroid inflammation by targeting thyroid tissue. While some individuals may experience increased thyroid activity initially, hypothyroidism can develop over time. Interestingly, those who develop thyroid issues during immunotherapy have shown higher cancer survival rates, highlighting the complex interplay between cancer treatments and thyroid function.
Management of Hypothyroidism
Individuals who develop hypothyroidism due to cancer treatments often require lifelong thyroid hormone therapy to maintain proper hormone levels and energy metabolism. Levothyroxine, a synthetic thyroid hormone, is commonly prescribed to regulate thyroid function. Maintaining adequate thyroid hormone levels can not only alleviate hypothyroidism symptoms but also reduce the risk of cancer recurrence, particularly in thyroid-related cancers.
Cancer treatments can have a profound impact on thyroid health, leading to the development of hypothyroidism. Understanding the risks associated with various treatments, such as radiation therapy, surgery, hormone therapy, and immunotherapy, is essential in managing thyroid function post-cancer treatment. Regular monitoring and appropriate interventions can help mitigate the effects of cancer treatments on the thyroid gland, ensuring optimal health outcomes for cancer survivors.