Recent research conducted at UVA Cancer Center has shown that a second-generation melanoma vaccine has significantly improved long-term survival rates for melanoma patients in comparison to the first-generation vaccine. This new vaccine has proven to be particularly beneficial for male patients, raising important questions about the implications for the development of other cancer vaccines in the future.
Enhanced Immune Response
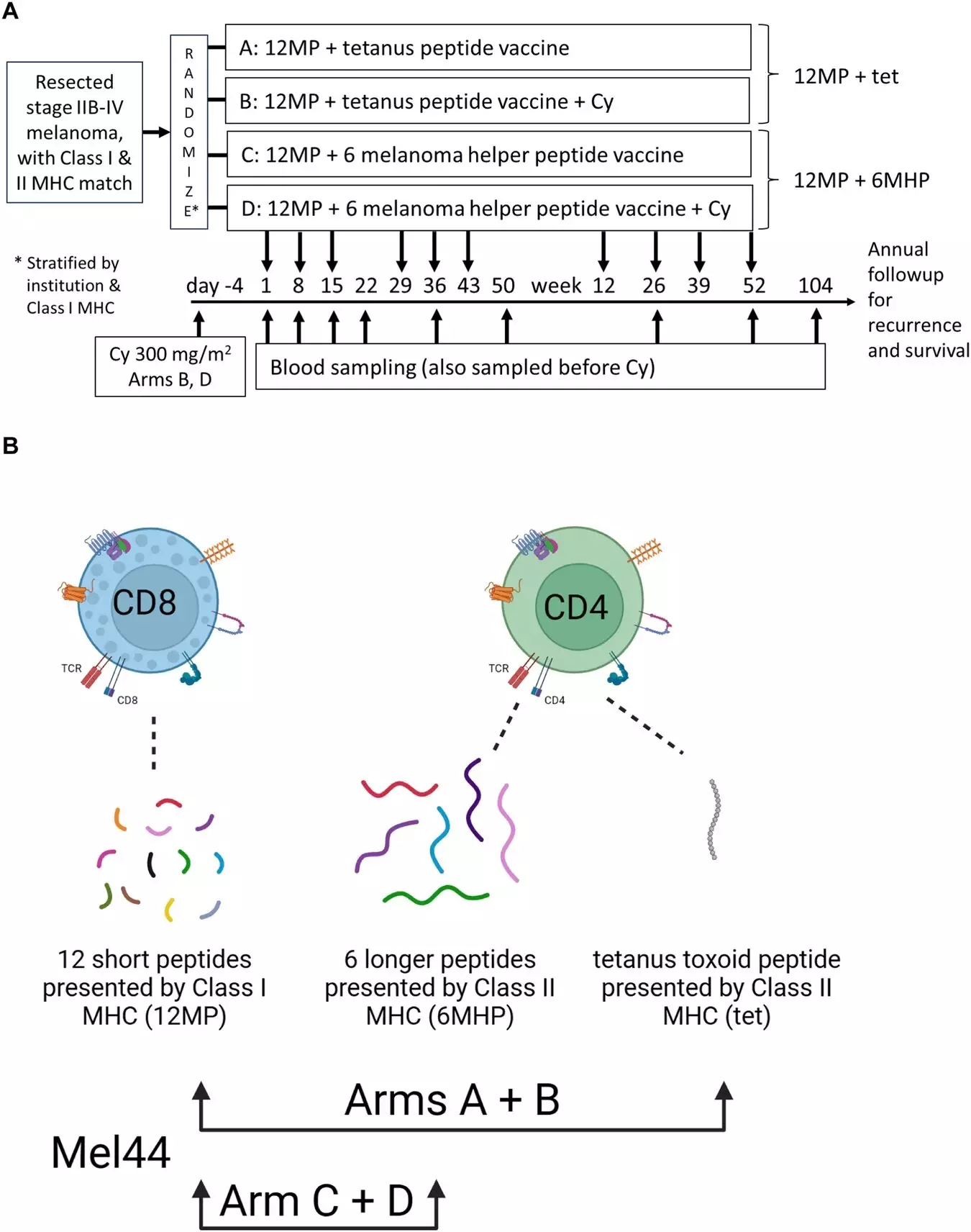
Led by Craig L. Slingluff Jr., MD, the team of vaccine developers discovered that by simultaneously stimulating helper T cells and killer T cells to recognize melanoma proteins, they could enhance the effectiveness of their melanoma vaccine. This dual stimulation approach not only increased patient survival rates but also helped in preventing the reoccurrence of the cancer. The researchers are still uncertain about why this approach was more effective in men, but it underscores the growing significance of biological sex in determining the outcomes of patients undergoing immune therapies.
The results of this study highlight the importance of gaining a better understanding of how to best benefit both women and men with the use of effective immunotherapies. As Slingluff explains, the promising results of the second-generation melanoma vaccine offer hope for patients undergoing surgery for high-risk melanoma. When combined with other immune therapies, this vaccine has the potential to provide even greater benefits, surpassing the results of either treatment used in isolation.
Changing the Perception of Vaccines
In the context of cancer treatment, vaccines are typically associated with preventing viral infections. However, melanoma vaccines serve a different purpose by inducing immune responses against human melanoma cells. While most cancers do not have a viral cause, there are exceptions, such as cancers caused by the human papillomavirus and hepatitis B. Slingluff’s work on developing a melanoma vaccine aims to combat a form of skin cancer that annually claims the lives of thousands of Americans.
Future Directions and Collaborations
Throughout the course of the clinical trials, Slingluff and his team tested two different approaches to stimulating CD4+ helper T cells and CD8+ killer T cells in patients with high-risk melanoma. The results, published in a new paper, demonstrate a meaningful and durable benefit for patients who received the second-generation vaccine. The researchers are now exploring the potential of combining this vaccine with other immune therapies to further enhance the survival rates of melanoma patients.
The findings of the multicenter trial suggest that both age and sex play crucial roles in determining the outcomes of immune therapies. This information is vital for healthcare professionals and researchers working on the development of new treatments. Understanding the reasons behind these differences based on age and sex is key to ensuring that all patients, regardless of their demographic characteristics, can receive the same level of benefit from innovative immunotherapies.
The development of second-generation melanoma vaccines represents a significant step forward in improving patient survival rates and preventing cancer reoccurrence. By exploring the unique impacts of age and sex on immune therapy outcomes, researchers can tailor treatments to meet the specific needs of individual patients, ultimately leading to more effective and personalized cancer care.