Blood donation is a crucial component of healthcare, ensuring a steady supply of safe blood for those in need. Every potential donor undergoes a preliminary health assessment that evaluates vital indicators such as pulse, blood pressure, temperature, and hemoglobin levels. Hemoglobin, a protein found in red blood cells, plays a critical role in transporting oxygen throughout the body. If levels are found to be abnormal, further donation may either be delayed or completely halted, as low hemoglobin can be symptomatic of various underlying health issues, including anemia or even leukemia.
This initial assessment serves as a critical screening tool, filtering out individuals who may have health conditions that could complicate their ability to donate safely. However, while the process is thorough, it traditionally does not include specific tests for leukemia unless anomalies are detected during routine evaluations.
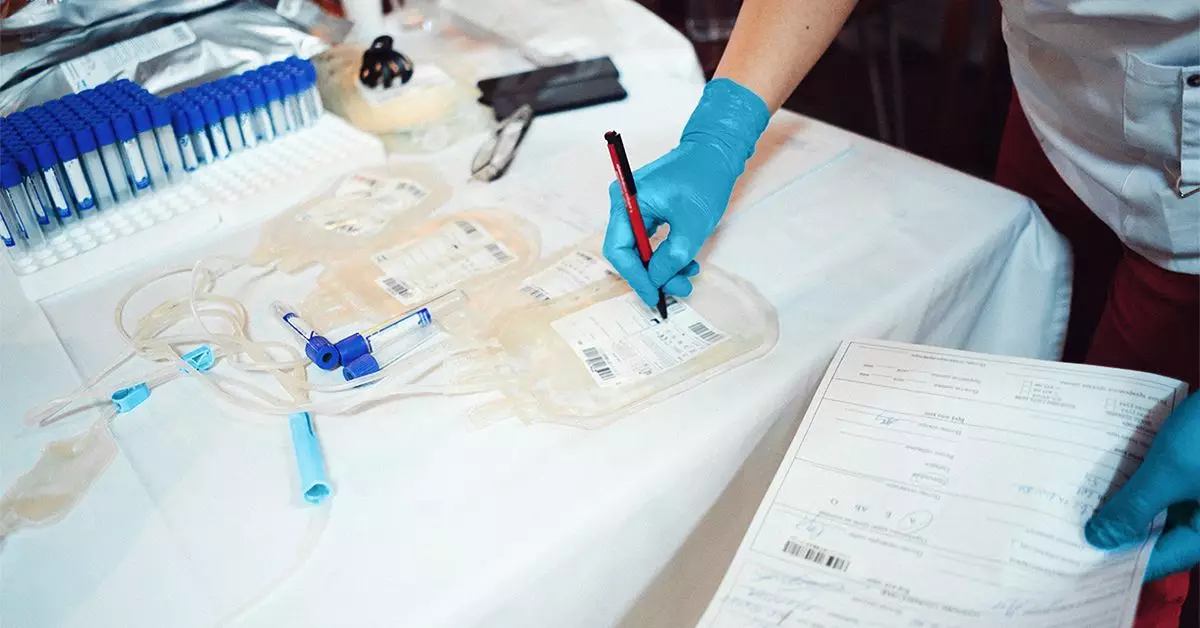
The standard blood donation protocols encompass a broad range of testing for infectious diseases, blood type, and other health markers. Yet, it is essential to note that leukemia is generally not a focus of standard testing. Although rare, certain conditions like HTLV-1 can lead to adult T-cell leukemia (ATL), drawing a connection between viral infections and blood cancers. If a potential donor is found to carry markers indicative of such conditions, the blood is promptly discarded, and the individual may be notified.
While this testing framework addresses immediate safety concerns, there remains a significant gap in proactive leukemia screening. The connection between donated blood and potential health issues like leukemia often arises when unexpected results surface during the processing phase, prompting further investigation.
When abnormalities are detected in donated blood, healthcare professionals play a vital role in informing donors. This system not only ensures the safety of the blood supply but also encourages donors to seek further medical evaluation. Awareness of one’s health status is crucial, and potentially alarming findings should be followed up with a healthcare provider to rule out serious conditions like leukemia.
Moreover, individuals with a historical diagnosis of leukemia are excluded from the blood donation pool. This regulation is vital for the safety of both patients relying on transfusions and the donors themselves, as active or recovered leukemia can complicate the health implications of donating blood.
While blood donation is an invaluable service in the medical community, the protocols surrounding it have limitations that may overlook conditions like leukemia. The routine assessments serve a crucial purpose, but advancing the dialogue surrounding testing methodologies is necessary to ensure a more comprehensive safety net for donors and recipients alike. Awareness and education about potential risks, alongside stringent follow-up actions, are keys to improving not just donor health, but public confidence in the blood donation system.